Introduction
Urgent care billing supports quick, accurate, and compliant payment cycles for clinics that handle high-volume walk-ins, sudden medical needs, short consultations, minor injuries, lab tests, and diagnostic procedures. A strong urgent care billing structure creates smooth financial operations, predictable revenue flow, error-free documentation, and clean payer communication. The system becomes more efficient when urgent care billing services, Urgent Care RCM, urgent care EHR, Urgent Care Revenue Cycle Management, and urgent care CPT coding operate in perfect alignment.
Role of Urgent Care Billing
Urgent care billing plays a vital part in helping clinics convert patient visits into timely payments. With proper workflows, clinics reduce administrative struggles, claim errors, payer delays, and reimbursement loss. Urgent care billing supports chart review, charge creation, coding validation, insurance checks, payment posting, denial correction, and ongoing financial reporting. With a growing patient count, fast turnaround becomes extremely important for daily cash flow. A structured urgent care billing system prevents revenue leakage and supports long-term stability.
Urgent Care Billing Services Explained
Urgent care billing services offer complete support from patient registration to final payment reimbursement. These services include:
Patient eligibility checks
Chart documentation review
Charge entry
urgent care CPT coding
Claim creation
Claim submission
Denial resolution
Payment posting
AR follow-up
Monthly reporting
A specialized team managing urgent care billing services ensures accuracy throughout the process. Clinics gain improved collections, fewer rejections, cleaner data, faster payout cycles, and stronger compliance. Expert knowledge supports critical processes that influence financial outcomes.
Importance of Urgent Care RCM
Urgent Care RCM refers to the complete financial journey from patient visit to reimbursement. A strong RCM structure creates clarity, speed, and reliability inside the clinic. Urgent Care RCM handles scheduling, documentation validation, coding selection, claim preparation, payer coordination, AR follow-up, denial management, and compliance checks.
With more clinics facing claim rejections due to coding errors or incomplete documentation, Urgent Care RCM becomes essential for smooth operations. A high-performing RCM process boosts collections, supports financial transparency, and protects clinics from reimbursement risks.
Role of Urgent Care EHR in Billing
Urgent care EHR tools support providers with real-time documentation, structured templates, visit histories, diagnosis details, procedure notes, test results, and clinical summaries. These digital records directly influence the billing cycle because claims require complete clinical data.
An efficient urgent care EHR reduces omissions, documentation gaps, coding conflicts, and claim inconsistencies. When urgent care EHR integrates with billing systems, information flows smoothly without manual errors. This connection improves accuracy for charge entry, urgent care CPT coding, claim submission, and financial reporting.
Urgent Care Revenue Cycle Management Workflow
Urgent Care Revenue Cycle Management covers several connected stages:
1. Patient Registration
Staff collect demographic details, insurance information, visit reasons, and clinical concerns. Accurate data ensures no mismatches during claim submission.
2. Eligibility Verification
Insurance coverage confirmation determines patient responsibility, copay amount, and payer rules.
3. Clinical Documentation
Providers complete detailed documentation in the urgent care EHR. Every detail supports proper coding.
4. urgent care CPT coding
Certified coders assign CPT codes for procedures, evaluations, tests, and treatments. Correct urgent care CPT coding protects clinics from payer audits, revenue delays, and compliance issues.
5. Charge Entry
Billing teams create charges from clinical documentation.
6. Claim Submission
Claims go electronically to payers. Clean claims reach payers faster with fewer issues.
7. Payment Posting
Payer responses enter the billing system. Accurate posting helps clinics track financial status.
8. Denial Management
Billing teams analyze denial reasons, make corrections, and resubmit claims quickly.
9. AR Follow-Up
Teams regularly check unpaid claims, confirm payer status, communicate with insurance representatives, and recover pending amounts.
10. Reporting
Financial reports highlight denial patterns, revenue performance, coder accuracy, and workflow efficiency. Clinics make decisions using these insights.
This complete Urgent Care Revenue Cycle Management structure ensures predictable revenue performance.
Urgent Care CPT Coding Guidelines
Urgent care CPT coding requires deep knowledge of clinical procedures, medical necessity standards, testing rules, and documentation accuracy. Common coding categories include:
Evaluation visits
Minor injuries
X-rays
Injections
Splinting
Wound repair
Lab testing
Preventive care
Follow-up care
Correct urgent care CPT coding supports revenue protection. Frequent errors include lack of documentation, improper code selection, missing modifiers, and outdated code usage. Coders must stay updated with AMA guidelines, payer policies, and compliance requirements.
Technology Support for Urgent Care Billing
Digital tools improve billing efficiency through:
Automated claim scrubbing
AI-based coding suggestions
Real-time EHR data syncing
Error-detection alerts
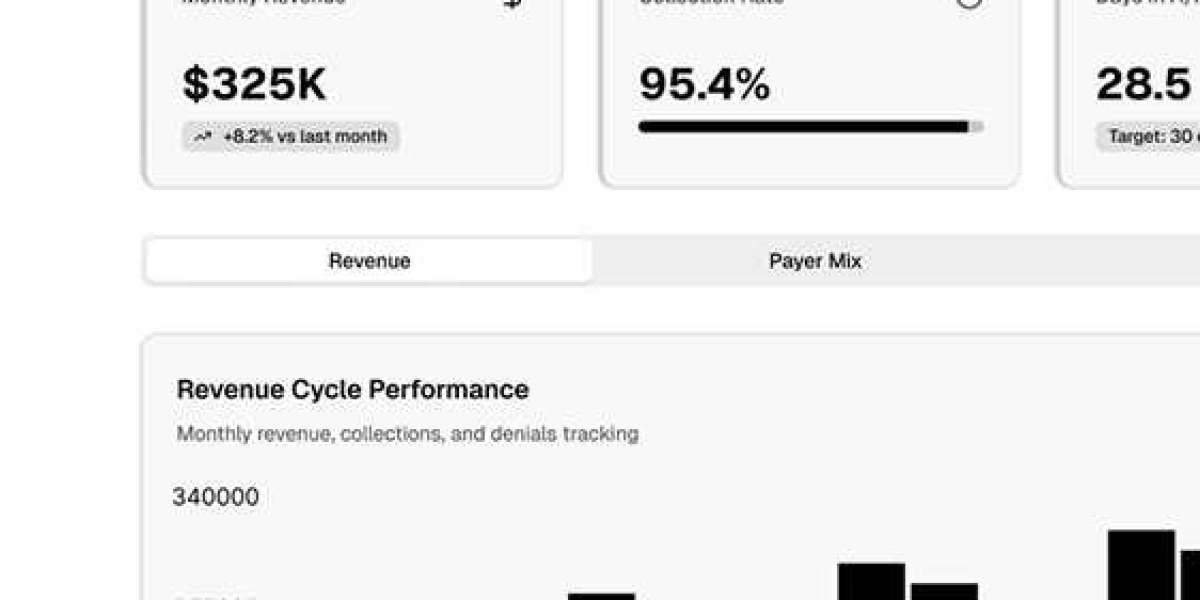
Performance dashboards
Online patient payments
Technology removes repetitive tasks, reduces documentation flaws, improves accuracy, and strengthens workflow speed. Clinics benefit from lower rejection rates and cleaner financial records.
Benefits of Outsourcing Urgent Care Billing Services
Outsourcing urgent care billing services offers value such as:
Higher revenue
Better coding accuracy
Faster claim turnaround
Full denial analysis
Zero administrative overload
Lower operational cost
Continuous support
Strong compliance monitoring
Outsourcing frees clinical teams from paperwork, so providers can focus on patient care. Billing experts manage coding, payer rules, and compliance without gaps.
Conclusion
Urgent care billing becomes the foundation of financial success for medical clinics. Strong urgent care billing services support accurate documentation, correct urgent care CPT coding, efficient claim creation, smooth claim submission, and powerful Urgent Care Revenue Cycle Management. Integrated urgent care EHR keeps documentation complete and error-free. With proper Urgent Care RCM, clinics gain improved revenue outcomes, faster reimbursements, lower denial rates, clean financial reports, and long-term operational stability.