Endothelial tissue refers to the blood vessel lining serving as a barrier. Its ubiquitous presence ranges from cardiac tissue to the smallest vessels. It coordinates several processes in physiology and disease. The role of the endothelium has been extensively explored in cardiovascular research. However, its involvement in inflammation has extended its research in various disorders, especially tumors. This blog details the Endothelial Tissue, its functions, and types.
Endothelial Tissue
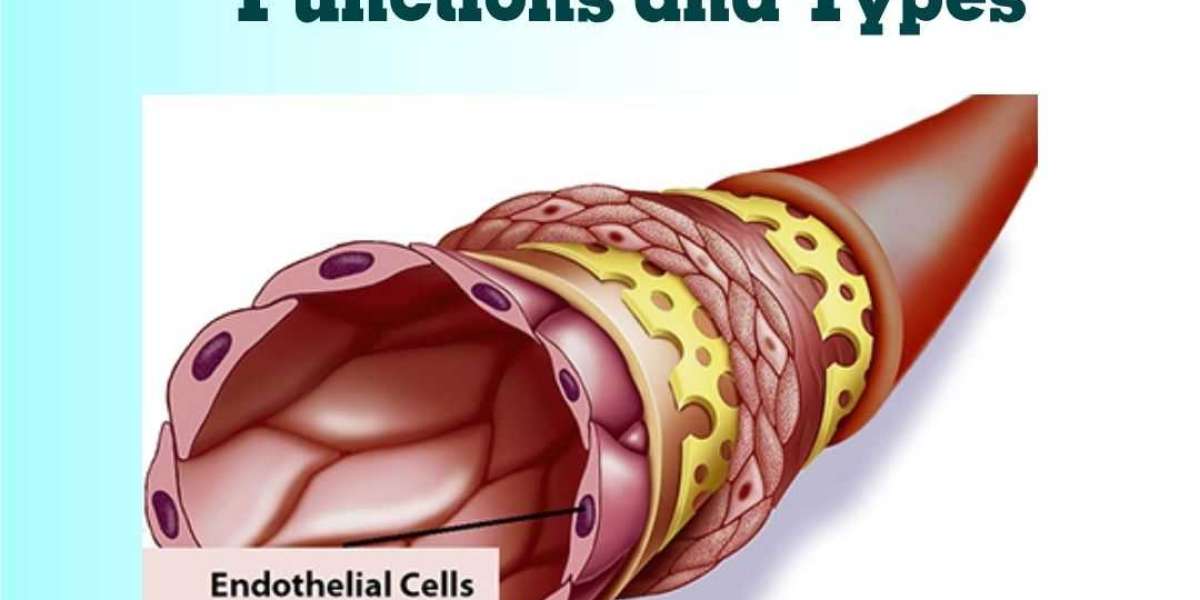
Endothelial tissue is present as a monolayer of polygonal cells on the luminal side of the vessel. In cell culture, endothelial cells (ECs) display a cobblestone pattern and express characteristic markers- von Willebrand factor (vWF), CD31, Weibel-Palade bodies, CD34, and VE-cadherin.
They typically have a basement membrane followed by layers of smooth muscle. The structure of the tissue alters depending on the tissue association and physiological factors. Modifications in their genome and proteome grant them a distinct signature and behavior.
Endothelial Tissue Function
The growing research has revealed and considerably expanded the Endothelial Tissue Functions.
Barrier
ECs are connected via different junctions- gap, adherent, and tight. They form a monolayer that regulates the traffic between blood and tissue. The permeability of this barrier varies with the tissue type. The significance of the barrier is most prominent in the brain. The tight junctions create an almost impermeable barrier across the brain. It prevents the entry of pathogens and toxins into the brain. However, at the time of injury, the endothelial barrier increases its permeability to allow immune cell migration. Loss of barrier property can eventually lead to edema.
Hemostasis
In case of injury, platelets migrate to the injury site and form a fibrin clot. This process involves complex interactions between ECs and platelets. ECs release von Willebrand factor (vWF), which binds to exposed extracellular matrix, stabilizes factor VIII, and enables interaction between platelet and tissue via glycoprotein receptor. It also produces platelet-activating factor (PAF) that stimulates platelet adhesion to the endothelium. Platelet release mediators, in response to which endothelium secretes nitric oxide (NO) and prostacyclin to prevent thrombosis.
Vascular Tone
Endothelium maintains an anti-coagulant state in normal circumstances. In addition to prostacyclin and NO secretion, ECs also express thrombomodulin that converts thrombin to an anticoagulant enzyme, thus preventing coagulation. Additionally, ligand-bound thrombomodulin activates protein C. Protein C and protein S together inactivate key factors involved in clot formation. Heparin-like glycosaminoglycans on the endothelial surface activate anti-thrombin, while tissue-factor pathway inhibitor (TFPI) inactivates the complex of tissue factor and factor VIIa, involved in coagulation.
Fibrinolysis
Dissolving the clot after injury repair is a vital step. ECs release two key proteins, tissue-type plasminogen activator (t-PA) and urokinase-type plasminogen activator (u-PA). While t-PA is constitutively present in the endothelium and released upon stimulation, u-PA is synthesized upon endothelial cell activation. Both convert proenzyme, plasminogen, into plasmin, which degrades fibrin. Additionally, ECs release plasminogen activator inhibitor-1 (PAI-1) that inhibits t-PA and u-PA. Increased PAI-1 is correlated with a higher risk of cardiovascular disorders. ECs maintain the balance between both for proper repair and blood flow.
Adhesion
Injury triggers an inflammatory cascade that recruits immune cells to the injury site. ECs are essential in this mechanism. They upregulate integrins, selectins, and cell adhesion molecules (CAMs), which bind to immune cells and facilitate their migration. Additionally, the endothelium allows the transport of immune cells into the tissue via paracellular or transcellular pathways.
Blood Flow
ECs face shear stress from increased blood flow. They orient themselves to decrease resistance and adapt to the stress. Moreover, they also release vasodilators such as PGI2, eNOS, and EDRF. Shear stress also stimulates ECs to suppress smooth muscle cell proliferation, leukocyte adhesion, and coagulation. The non-adherent, anti-coagulative surface of endothelium functions to support the normal blood flow.
Angiogenesis
Angiogenesis occurs during body growth and injury repair. It entails the degradation of the extracellular matrix to enable the proliferation and migration of ECs to develop tubular structure. ECs release factors such as angiopeptin-2, VEGF, IGF1, FGF2, matrix metalloproteinases (and their inhibitors), etc., to regulate the process tightly.
Endothelial Tissue Types
ECs show considerable heterogeneity in their phenotype, functions, and properties. It has categorized three endothelial tissue types as under-
Arterial ECs: ECs in arteries are narrower and elongated to adapt to the high shear stress. The blood vessels have a thicker smooth muscle cell layer to accommodate the blood pressure.
Venous ECs: The cells are shorter and wider, along with relatively fewer layers of smooth muscle cells, owing to the low blood flow rate.
Capillary ECs: This endothelial layer is thin for efficient gaseous and nutrient exchange.
Lymphatic ECs: Due to their role in immune response, ECs of the tissue have a thin, discontinuous membrane with button-like junctions.
Endothelial tissue types can also be categorized based on the organ they are associated with, such as the brain, liver, and kidney. Another classification of endothelial tissue types depends on their permeability: continuous (tight barrier), fenestrated (contains pores), and discontinuous (gaps between cells).
Conclusion
Endothelial tissue is widespread in the body. In a static state, it might only display the barrier function. However, looking closely, one can find that maintaining the static barrier is also complex. It delicately balances numerous processes to sustain a healthy state. Any dysfunction can lead to severe medical disorders. Therefore, endothelium has found applications in basic research and disease studies. Kosheeka, a GMP-compliant company, offers endothelial cells at low passage numbers to assist researchers in their subsequent discovery.